Neonatal Pneumothorax in Late Preterm and Full-Term Newborns with respiratory Distress: A Single-Center Experience
Article information
Abstract
Purpose
To evaluate the incidence rate, clinical characteristics, and perinatal outcomes of pneumothorax in late preterm and full-term newborns with respiratory distress and analyze the risk factors associated with pneumothorax.
Methods
Infants born at ≥34 weeks’ gestation with respiratory distress and pneumothorax admitted between February 2014 and December 2020 were enrolled in this study. The pneumothorax group (n=36) was matched to the control group (n=144) in a 1:4 ratio, based on gestational age and birth weight. Risk factors were identified using logistic regression analysis with backward stepwise selection.
Results
The incidence of pneumothorax during the study period was 1.36% (38/2,788). All patients were diagnosed with pneumothorax within 48 hours after birth, and increased oxygen demand was the most common symptom. The proportion of mortality and perinatal morbidity, such as intraventricular hemorrhage ≥grade 3, was significantly higher in the pneumothorax group than in the control group. The risk factors associated with pneumothorax were the need for positive pressure ventilation in the delivery room (odds ratio [OR], 3.40; 95% confidence interval [CI], 1.26 to 9.12; P=0.015) and a higher fraction of inspired oxygen to achieve an oxygen saturation of ≥90% on admission (OR, 1.06; 95% CI, 1.03 to 1.09; P<0.001).
Conclusion
Pneumothorax should be suspected in late preterm and full-term newborns with respiratory distress within the first 3 days of life. Based on these risk factors, early diagnosis can reduce perinatal mortality and morbidity.
INTRODUCTION
Pneumothorax, a common air leak syndrome in the neonatal period, is defined as abnormal air accumulation between the visceral and parietal pleura. It can increase intrathoracic pressure, resulting in partial or complete collapse of the lung on the affected side. The clinical manifestation of pneumothorax depends on the degree of collapse of the lung, which can impair pulmonary gas exchange and hemodynamic stability and may result in a life-threatening condition. Pneumothorax occurs more frequently in newborns than in any other age group, with an incidence rate of 1% to 2% in the general population and 6% to 7% in very low birth weight (VLBW) infants with a birth weight of less than 1,500 g [1-3]. Moreover, symptomatic pneumothorax occurs in 0.08% of all live births and 5% to 7% of VLBW infants [4].
Despite advances in neonatal intensive care, such as the use of antenatal steroids, surfactant replacement therapy, and lung-protective ventilator strategies, pneumothorax remains a common respiratory complication that contributes to an increase in perinatal morbidities, including intraventricular hemorrhage (IVH), bronchopulmonary dysplasia (BPD), and mortality, especially in preterm infants and critically ill newborns [5-7]. Although prematurity and respiratory distress syndrome (RDS) have been considered important contributing factors associated with pneumothorax, pneumothorax frequently occurs in all newborns who have underlying lung disease or require either noninvasive or invasive mechanical ventilation [8,9]. Late preterm and term newborns with neonatal pneumothorax are usually asymptomatic, but patients with respiratory distress tend to be symptomatic, resulting in acute respiratory failure or life-threatening condition [1]. Pneumothorax occurring in term infants with respiratory distress is also associated with increased morbidities and length of hospitalization [10]. Many previous studies on neonatal pneumothorax have focused on early preterm newborns; therefore, further studies on the epidemiology, clinical characteristics, and risk factors of pneumothorax in late preterm and full-term newborns are required.
This study aimed to evaluate the incidence of pneumothorax in late preterm and full-term newborns with respiratory distress and compare the clinical characteristics, perinatal morbidities, and mortality between late preterm and full-term newborns with and without pneumothorax during hospitalization. Moreover, we aimed to identify the risk factors associated with pneumothorax in late preterm and full-term newborns with respiratory distress.
MATERIALS AND METHODS
1. Study population and design
We retrospectively reviewed the electronic medical charts of all newborns admitted to the neonatal intensive care unit (NICU) of Kyungpook National University Chilgok Hospital (KNUCH) between February 2014 and December 2020. This retrospective case-control study was approved by the Institutional Review Board of KNUCH, with a waiver of consent (2021-10-003).
Neonatal pneumothorax was defined as abnormal air accumulation between the visceral and parietal pleura within 28 days after birth or at 44 weeks of corrected gestational age (GA). Pneumothorax was classified as spontaneous/secondary, unilateral/bilateral, and tension/non-tension pneumothorax. Spontaneous pneumothorax was defined as pneumothorax that developed without apparent causes, including predisposing factors (intubation or positive pressure ventilation [PPV]) and underlying lung diseases, while secondary pneumothorax with traumatic injury to the pleura and underlying lung diseases [11]. Underlying lung diseases included RDS, transient tachypnea of the newborn (TTN), meconium aspiration syndrome (MAS), congenital pneumonia, and congenital lung hypoplasia. Tension pneumothorax was defined as compromised cardiopulmonary function with a mediastinal shift in unilateral or diaphragmatic depression in bilateral pneumothorax [11]. The treatment of neonatal pneumothorax in the NICU of KNUCH is as follows: (1) close observation with or without 100% supplemental oxygen administration, (2) needle aspiration, and (3) intercostal drainage (closed thoracostomy). Management strategies for neonatal pneumothorax depend on the hemodynamic stability of the infants. Newborns with asymptomatic pneumothorax or mild respiratory distress were closely observed with or without administration of 100% supplemental oxygen. If newborns had tension pneumothorax or aggravated cardiopulmonary symptoms, needle aspiration or intercostal drainage was performed immediately by experienced thoracic surgeons or neonatologists. The intercostal drainage was removed if the patient showed improvement in symptoms and signs of pneumothorax clinically and radiologically.
The inclusion criteria for the case group (pneumothorax group) were as follows: (1) infants with a GA of ≥34 weeks and admitted to the NICU due to respiratory distress and (2) infants diagnosed with pneumothorax on chest radiograph during hospitalization. Infants with life-threatening congenital malformations were excluded from this study. Four controls matched for GA and birth weight were selected from infants with a GA of ≥34 weeks who were admitted to the NICU of KNUCH due to respiratory distress during the study period. We analyzed the incidence rate and described the clinical manifestations at the onset and management of the pneumothorax group. We compared demographic and clinical characteristics, resuscitation in the delivery room, respiratory support on admission, perinatal morbidities, and mortality between the pneumothorax and control groups. We also evaluated the risk factors associated with pneumothorax in newborns born with a GA ≥34 weeks and respiratory distress.
2. Variables
The demographic and clinical characteristics were as follows: GA based on the maternal last menstrual period, modified Ballard score, obstetric ultrasonography results, birth weight, Apgar score at 1 and 5 minutes, delivery mode, gender, small for gestational age (SGA), maternal premature rupture of membranes, oligohydramnios, pregnancy-induced hypertension, gestational diabetes mellitus, and the use of antenatal steroids [12]. SGA is defined as a birth weight below the 10th percentile for GA [13]. Oligohydramnios refers to a decrease in amniotic fluid volume for GA, along with an amniotic fluid index <5 cm [14].
Data on resuscitation in the delivery room and respiratory support on admission were collected. Neonatal resuscitation in the delivery room included PPV, intubation, chest compression, and continuous positive airway pressure (CPAP) during transport to the NICU. Respiratory support on admission included a highflow nasal cannula (HFNC), nasal CPAP, mechanical ventilation, fraction of inspired oxygen (FiO2) to achieve an oxygen saturation (SPO2) of ≥90%, and surfactant administration.
The clinical features and respiratory support in infants with pneumothorax at diagnosis were as follows: onset time (hours after birth), symptoms, location (right and left), tension pneumothorax, respiratory support at onset (HFNC, nasal CPAP, mechanical ventilation, maximum positive expiratory end pressure [PEEP], maximum mean airway pressure [MAP], maximum FiO2 to achieve an oxygen saturation of ≥90%), management (close observation, 100% supplemental oxygen administration, needle aspiration, intercostal drainage), and underlying pulmonary diseases such as RDS, TTN, MAS, and congenital pneumonia.
The perinatal outcomes included IVH with a Papile classifcation of ≥grade 3 [15], periventricular leukomalacia (PVL), moderate to severe BPD defined as the requirement of supplemental oxygen or positive pressure to maintain an oxygen saturation of ≥92% before discharge from the NICU or at 36 weeks of corrected GA [16], necrotizing enterocolitis ≥Bell’s stage IIb [17], sepsis-confirmed bacterial or fungal pathogens on blood culture, retinopathy of prematurity requiring treatment, duration of hospitalization, and death before discharge.
3. Statistical analysis
Continuous variables are presented as means and standard deviations, whereas categorical variables are presented as numbers and percentages (%). To compare the differences between the demographic clinical characteristics, resuscitation in the delivery room, respiratory support on admission, and perinatal outcomes between the two groups, Student’s t-test and MannWhitney test were used for continuous variables, and the chisquare test and Fisher’s exact test were used for categorical variables. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using logistic regression analysis to evaluate risk factors associated with neonatal pneumothorax. Backward stepwise selection was conducted to adjust for confounders owing to the retrospective nature of the present study. All statistical analyses were performed using SPSS version 26 (IBM Co., Armonk, NY, USA), and a P<0.05 was considered statistically significant.
RESULTS
1. Study population and the incidence of neonatal pneumothorax
Between February 2014 and December 2020, 3,406 newborns were admitted to the NICU of KNUCH because of respiratory distress, and 2,788 had a GA of ≥34 weeks. Among infants with GA ≥34 weeks, 38 (1.4%) were diagnosed with pneumothorax, and 32 (1.1%) were diagnosed with symptomatic pneumothorax requiring intervention, such as high-concentration oxygen (FiO2 100%), needle aspiration, and intercostal drainage. Two infants who died within 24 hours of birth due to life-threatening congenital malformations were excluded. Finally, the present study included 36 infants (13 men and 23 women) with pneumothorax and 144 infants as the control group, which matched the GA and birth weight with pneumothorax cases.
2. The demographic and clinical characteristics of the pneumothorax and control groups
Table 1 shows a comparison of the demographic and clinical characteristics of the pneumothorax and control groups. The mean GA and birth weight of the pneumothorax group were 37.9±2.0 weeks and 3,060±587 g, which were not statistically different compared with the control group (37.7±1.9 weeks of GA and 3,024±477 g of birth weight). The proportion of Apgar scores at 5 minutes <7 in the pneumothorax group (4/36, 11.1%) was significantly higher than that in the control group (1/144, 0.7%). Other demographic and clinical characteristics were not significantly different between the pneumothorax and control groups.
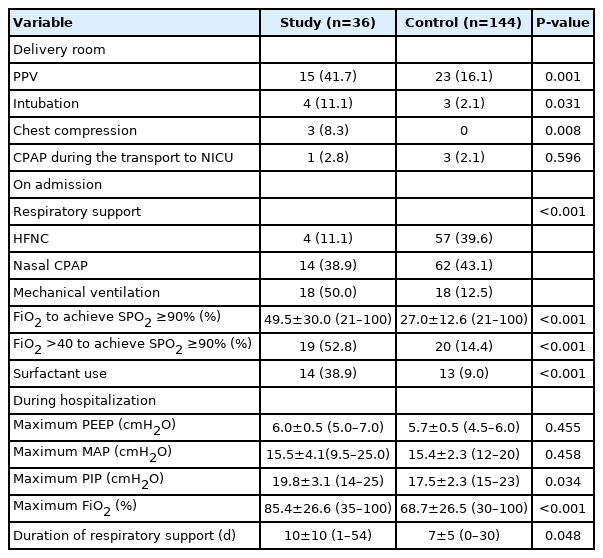
3. The resuscitation in the delivery room and respiratory support on admission of the pneumothorax and control group
Table 2 shows the data for resuscitation in the delivery room and respiratory support on admission in the pneumothorax and control groups. Cardiopulmonary resuscitation in the delivery room was more frequent in the pneumothorax group than in the control group; 15 (41.7%) and 23 (16.1%) infants received PPV in the pneumothorax and control groups, respectively (P=0.001); four (11.1%) and three (2.1%) infants received endotracheal intubation in the pneumothorax and control groups, respectively (P=0.041); and three (8.3%) and 0 (0.0%) infants underwent chest compression in the pneumothorax and control groups, respectively (P=0.035).
A statistically significant difference in respiratory support on admission was observed between the pneumothorax and control groups. The majority of infants with pneumothorax (32/36, 88.9%) required respiratory support on admission with nasal CPAP (14/36, 38.9%) and mechanical ventilation (18/36, 50.0%), although only approximately half of the control group (80/144, 55.6%) required respiratory support with nasal CPAP (62/144, 43.1%) and mechanical ventilation (18/144, 12.5%). The FiO2 to achieve SPO2 of ≥90% of the pneumothorax group (49.5%±30.0%) was significantly higher than that of the control group (27.0%±12.6%). The use of surfactants for RDS or MAS was more frequent in infants with pneumothorax than in those without pneumothorax (14/36 [38.9%] and 13/144 [2.0%] in the pneumothorax and control groups, respectively).
4. The clinical characteristics at onset of pneumothorax
Table 3 shows the clinical features and respiratory support data for the diagnosis of pneumothorax in newborns in the pneumothorax group. Thirty-six infants were diagnosed with pneumothorax presenting with respiratory distress symptoms (tachypnea, chest retraction, nasal flaring, cyanosis), hypercarbia, or increased supplemental oxygen concentration at a mean age of 20.2±14.8 hours of life. Among 34 (94.4%) infants who needed respiratory support at the onset of pneumothorax, 29 (80.6%) received CPAP (10/36, 27.8%) and mechanical ventilation. The mean maximum PEEP and MAP at the diagnosis of pneumothorax were 6.5±1.2 and 11.8±4.3 cmH2O, respectively. The mean FiO2 to achieve an oxygen saturation of ≥90% at the diagnosis of pneumothorax was 55.8%±31.6%. Thirty-two (88.9 %) infants had unilateral pneumothorax (right, n=23; left, n=9), and four (11.1%) had bilateral pneumothorax. Eleven (30.6%) patients experienced hemodynamic instability such as hypotension, low blood oxygen levels, and shock; consequently, they were diagnosed with tension pneumothorax. Twenty-four patients (66.7%) required needle aspiration (1/36, 2.8%) and intercostal drainage (23/36, 63.9%).
5. The final diagnosis for respiratory distress and perinatal outcomes of the pneumothorax and control groups
Table 4 shows a comparison of the final diagnosis and perinatal outcomes between the pneumothorax and control groups. A significant difference in underlying pulmonary diseases was observed between the pneumothorax and control groups. Infants who developed pneumothorax were predominantly diagnosed with spontaneous pneumothorax (30.6%), RDS (27.8%), and congenital pneumonia (16.7%); in contrast, three-quarters of the control group were diagnosed with TTN (76.4%).
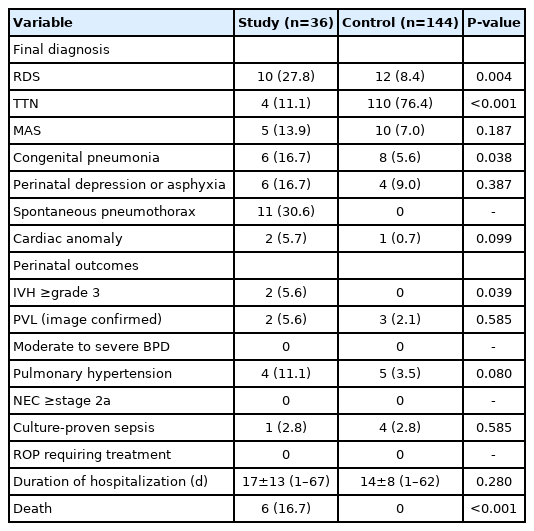
The Comparison of Perinatal Outcomes in Neonatal Intensive Care Unit between the Pneumothorax and Control Groups
In the comparison of perinatal outcomes, the incidence rate of grade ≥3 IVH (P=0.039) was significantly higher in the pneumothorax group than in the control group. The incidence rate of secondary pulmonary hypertension was higher in the pneumothorax group than in the control group, but the difference was not statistically significant (P=0.080). Other morbidities, including PVL, moderate to severe BPD, and culture-proven sepsis, were not significantly different between the pneumothorax and control groups. The duration of hospitalization was also not significantly different between the pneumothorax and control groups. Infants with pneumothorax had a significantly higher mortality rate than those in the control group (P<0.001); six infants in the pneumothorax group died during the study period.
6. The risk factors associated with pneumothorax in late preterm and full-term infants with respiratory distress
Table 5 shows the results of logistic regression with backward selection, which was conducted to determine the risk factors associated with neonatal pneumothorax. The need for PPV during resuscitation in the delivery room was significantly associated with neonatal pneumothorax (OR, 3.40, 95% CI, 1.26 to 9.12; P=0.015). However, the need for intubation was not significantly associated with neonatal pneumothorax (OR, 2.58; 95% CI, 0.27 to 24.39; P=0.407). A high requirement of FiO2 to achieve an SPO2 of ≥90% on admission was significantly associated with neonatal pneumothorax (OR, 1.06; 95% CI, 1.03 to 1.09; P<0.001).
DISCUSSION
This study aimed to compare the epidemiologic and clinical characteristics and perinatal outcomes between newborns with and without pneumothorax among late preterm and full-term newborns with respiratory distress on admission and determine the risk factors associated with neonatal pneumothorax. No significant differences in epidemiologic characteristics were observed except for the proportion of Apgar score at 5 minutes <7, but statistically significant differences in relation to the need for advanced neonatal resuscitation at birth and respiratory support on admission were observed between the pneumothorax and control groups. As expected, significantly higher rates of IVH (grade ≥3) and death during hospitalization were observed in infants with pneumothorax than in those in the control group. Based on the findings of this study, the use of PPV in the delivery room and a higher requirement of FiO2 to achieve an SPO2 ≥90% on admission were associated with neonatal pneumothorax in late preterm and full-term infants with respiratory distress.
The incidence rate of neonatal pneumothorax is 0.5% to 1% in the total population of live births [18]. A higher incidence rate of pneumothorax has been observed in critically ill newborns admitted to the NICU, and the incidence rate has been reported to vary from 1.5% to 13.5% [18-20]. In the present study, the overall incidence rate of neonatal pneumothorax was 1.36%, which was relatively low compared with that reported in previous studies. The incidence of neonatal pneumothorax is known to be associated with GA and birth weight, the proportion of elective cesarean section, and the severity of concurrent pulmonary disease [2,21-23]. Based on these findings, the differences in the incidence rates can be attributed to disparities in epidemiologic characteristics, severity of underlying lung disease in the study population, and institutional variation in ventilator strategies.
In the present study, late preterm and full-term newborns who developed pneumothorax needed advanced neonatal resuscitation, including PPV, intubation, and chest compression in the delivery room, as well as respiratory support on admission, such as nasal CPAP, mechanical ventilation, relatively high FiO2 to achieve an SPO2 of ≥90%, and the use of surfactants, more than those without pneumothorax. These results were consistent with the findings of previous studies. A retrospective populationbased descriptive study conducted in Sweden documented that 80% of term neonates with pneumothorax required PPV and/or endotracheal intubation at birth, as well as noninvasive and invasive respiratory support on admission [24]. A cohort study in Denmark also reported that nearly all newborns received nasal CPAP or an invasive mechanical ventilator prior to the onset of pneumothorax [22]. Indeed, the final diagnosis of respiratory distress was significantly different between the pneumothorax and control groups in this study. Newborns with pneumothorax are commonly diagnosed with RDS and congenital pneumonia, and more than three-quarters of infants without pneumothorax are confirmed to have TTN. Previous studies have also described that RDS, MAS, and congenital pneumonia were more common in infants with pneumothorax than in those without pneumothorax [24,25]. Some newborns with pneumothorax were diagnosed with TTN, but most cases of pneumothorax that occurred were asymptomatic and spontaneously resolved without treatment such as needle aspiration and intercostal drainage [22]. These findings suggest that late preterm and full-term infants who developed pneumothorax after birth were more likely to experience failure to cardiopulmonary transition from intra-uterine to extra-uterine environment and have serious underlying pulmonary disorders, including RDS, congenital pneumonia, or systemic conditions, including perinatal asphyxia, than those without pneumothorax.
Neonatal pneumothorax usually occurs within the first 3 days of birth in late preterm and term newborns [22,26]. Similarly, in the present study, all patients developed pneumothorax within the first 48 hours of life, with a mean onset time of 20.2 hours of life. These results were earlier than the onset time in early preterm infants born at <32 weeks of GA [2,27]. It has been suggested that pneumothorax in late-preterm and full-term newborns is mainly related to mechanical injuries of the lungs caused by trans-pulmonary pressure to maintain sufficient functional residual capacity at the initiation of breathing. In the first few minutes of life, the trans-pulmonary pressures averaged 40 cmH2O, and occasional pressures as high as 100 cmH2O were applied to the neonatal lung [28]. The clinical presentation of neonatal pneumothorax is nonspecific. In the present study, more than three-quarters of the patients had increased oxygen demand to maintain appropriate saturation, and half of the patients had tachypnea before being diagnosed with pneumothorax. In accordance with the results of the present study, a retrospective population-based descriptive study conducted in Orebro County reported that the common clinical presentations of neonatal pneumothorax were tachypnea (77%) and cyanosis (56%) [24]. However, these respiratory symptoms and signs cannot be distinguished from those of other neonatal pulmonary diseases including RDS and TTN. Therefore, careful attention should be paid to the development of pneumothorax in late preterm and full-term infants within the first 3 days of life, and appropriate examinations, including chest radiography or lung ultrasound, should be performed immediately if respiratory symptoms worsen, such as aggravated tachypnea and increased oxygen demand.
Neonatal pneumothorax is associated with increased perinatal morbidities. In the present study, infants who developed pneumothorax had significantly higher rates of severe IVH. Few studies have reported that neonatal pneumothorax is significantly associated with IVH and persistent pulmonary hypertension of the newborn (PPHN) [4,29]. These comorbidities were found to contribute to increased mortality in newborns with pneumothorax. Significantly higher mortality rates were observed in newborns who developed pneumothorax than in those without pneumothorax, in which mortality rates of neonatal pneumothorax have been reported to be between 16% and 65% [22,29-31]. In the present study, the mortality rate of the pneumothorax group was 16.7% (6/36), which was statistically significant compared to that of the control group. However, the most common immediate cause of death was not pneumothorax but underlying pulmonary disease or concomitant neonatal morbidities [22,29-31]. The deaths of the pneumothorax group in the present study were directly caused by unresponsive PPHN in three cases, severe IVH in two cases, and multi-organ dysfunction related to severe perinatal asphyxia in one case. Therefore, proper management of underlying pulmonary diseases and concomitant morbidities associated with pneumothorax is important to reduce mortality in infants with pneumothorax.
For early detection of neonatal pneumothorax, it is necessary to determine the risk factors associated with pneumothorax and identify high-risk groups. Zanardo et al. [23] found that elective cesarean section before 39 weeks of GA resulted in an increase in the incidence of neonatal pneumothorax. Many previous studies have focused on respiratory support, especially pressure support, during resuscitation or before the diagnosis of pneumothorax. A Canadian retrospective cohort study and a Japanese study showed that CPAP use during neonatal resuscitation was a risk factor for pneumothorax in late preterm and full-term neonates [2,32]. A study on the birth cohort of the Parkland Health and Hospital System showed that the incidence rates of pneumothorax significantly increased in early full-term neonates after the introduction of CPAP in the neonatal resuscitation program [33]. The high maximum peak inspiratory pressure during the 24 hours before the detection of pneumothorax and clinical procedures, including suction procedures and reintubation, have also been associated with the occurrence of pneumothorax [29,31,34,35]. The present study found that the need for PPV in the delivery room and high FiO2 on admission were associated with neonatal pneumothorax with an OR of 3.40 (95% CI, 1.26 to 9.12; P=0.015) and 1.06 (95% CI, 1.03 to 1.09; P<0.001). Overall, these findings suggest that underlying lung disease with low compliance and interventions applying additional pressure above the average transpulmonary pressure during respiratory transition and damage to the airways and lungs caused by invasive procedures during the first few days of life were considered important risk factors associated with pneumothorax in late preterm and full-term newborns with respiratory distress. Based on these findings, continuous monitoring of respiratory distress and follow-up chest radiography after birth are thought to help detect pneumothorax early in late preterm and term infants, who require advanced neonatal resuscitation (PPV, intubation, and chest compression) and relatively high oxygen concentration to achieve an SPO2 of ≥90%. However, the findings of some studies on the risk factors affecting the development of pneumothorax in late preterm and full-term newborns are still inconsistent. Further large-scale and well-designed studies on the risk factors associated with neonatal pneumothorax are needed.
However, the present study has some limitations. First, this study had a retrospective design that depended on chart reviews, and the number of study populations was small because the present study was conducted in a single center. Second, chest radiography is not routinely performed in newborns without symptoms or signs of respiratory distress. The actual incidence of neonatal pneumothorax could have been underestimated due to the missing diagnosis of asymptomatic neonatal pneumothorax. Third, potential confounders included variations in neonatal resuscitation programs in the delivery room between inborn and out-born infants and insufficient data on the maternal or prenatal characteristics of out-born infants.
In conclusion, pneumothorax frequently develops in late preterm and full-term newborns with respiratory distress and is associated with high mortality and morbidity. Therefore, late preterm and full-term newborns with respiratory distress, especially those who required PPV to initiate breathing at birth and had relatively high oxygen concentrations to maintain appropriate oxygen saturation, should be meticulously followed up to monitor their respiratory conditions during their first 3 days of life. Furthermore, additional well-designed, prospective, controlled studies are needed to better predict and detect early neonatal pneumothorax in late preterm and full-term newborns with respiratory distress.
Notes
Ethical statement
The institutional Review Board of the Kyungpook National University Chilgok Hospital approved the study (IRB No. 2021-10-003). Informed written consent was waived due to the retrospective design of the study.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design: J.S.K.
Acquisition, analysis, or interpretation of data: E.A.K., J.H.J., S.Y.L., J.S.K.
Drafting the work or revising: E.A.K., J.S.K.
Final approval of the manuscript: All authors read and approved the final manuscript.
Funding
None
Acknowledgements
None