|
 |
- Search
| Neonatal Med > Volume 30(1); 2023 > Article |
|
Abstract
In 2004, the Neonatal Research Network of Japan initiated a database registration system for high-risk infants in Japan. Currently, 65% of all very low the birth weight infants or infants born at <32 weeks of gestation are registered in the database. Approximately 4,000 new cases are registered annually. A unique feature of the database is that it includes outcome data at 1.5, 3, and 6 years after discharge from neonatal intensive care units. All registered data are fed back annually to the participating hospitals and used to benchmark neonatal care. Results from this database have also been published in many international journals. With the development of this database, neonatal medicine in Japan has progressed.
The Neonatal Research Network of Japan (NRNJ) was established in 2003 by a research group (principal investigator: Masanori Fujimura) of the Japanese Ministry of Health, Labour and Welfare science research project, titled "Perinatal Center Network" [1,2]. In the following year, the NRNJ created a database of high-risk infants. The basic database structure was discussed and decided upon by this research group, and actual data registration started from infants born in 2003 with a birth weight of Ōēż1,500 g. Infants born before 32 weeksŌĆÖ gestation were included in 2015. The current database comprises 156 variables for infants. All data are collected until discharge from the neonatal intensive care unit (NICU). In addition to the variables in the NICU, the database also collects follow-up data at 1.5, 3, and 6 years of age. This is a unique feature of the database compared with other existing databases.
The first objective of the study was to improve neonatal care for high-risk infants, and determining and evaluating the current status of their outcomes as the first step necessary. Otherwise, the steps necessary to improve the outcomes cannot be clarified. Once the actual figures of the outcomes become clear, the measures to be taken to improve the outcomes will also become apparent.
The second objective was to use a database for benchmarking and quality improvement. Learning from high-performance centers is generally effective in improving the outcomes of the entire network. These activities can also lead to the standardization of neonatal intensive care.
The last objective was to provide opportunities for clinical research using databases.
The network database project was supported by a grant from the Japanese Ministry of Health, Labour, and Welfare from 2004 to 2011. However, since 2014, the NRNJ has been operating with support from academic societies, such as the Japan Society of Neonatal Medicine and Development and the Japan Society for Perinatal and Neonatal Medicine and from donations.
Participation in the network database is voluntary. Japan has approximately 100 level III and 300 level II perinatal centers. When the database was launched in 2003, only 40 perinatal centers participated. Since then, the number of participating hospitals has increased, with approximately 170 participating hospitals [3]. However, approximately half of all participating hospitals are level III perinatal centers, indicating that relatively large-scale level III perinatal centers predominantly participated among all perinatal centers. The database covers approximately 65% of the total population of high-risk infants born in Japan.
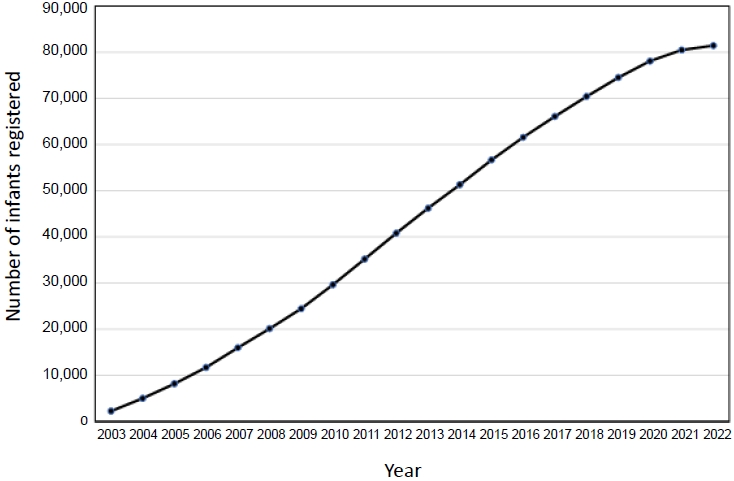
All necessary data can be registered on a designated website. All items during the NICU stay should be uploaded immediately after discharge from the NICUs. Figure 1 presents the cumulative number of infants registered in the database. Currently, >80,000 infants have been registered. When a medical follow-up examination is performed at the ages of 1.5, 3, and 6 years after discharge from the NICUs, follow-up information can be registered on the same website. Because all registered variables are stored as numerical and text data with a center-specific identifier (ID), decrypting the data content is not possible, even if a third party downloads the data. Furthermore, even if the data structure is clarified, identifying the individual would not be possible as personally identifiable information, such as date of birth, is not registered initially, and hospital identifications are all dummy numbers.
The registered data were aggregated, and feedback was provided to the participating hospitals once a year. The content of the input includes the summarized results of all participating centers and the data unique to each center. The ranking of each hospital can be determined by the number of centers provided in the feedback. Each center can identify its rank as a benchmark.
Until 2016, these feedback data were printed and distributed to participating hospitals as annual reports; however, all feedback data could be downloaded as portable document format (PDF) files from the website. Aggregated data have also been published on the website.
Since 2007, quality improvement conferences have been held yearly by gathering representatives from participating hospitals. In the conference, strategies to reduce center variations, trends in mortality and morbidities, prevention of major morbidities, and improvement of database items and annual database analysis reports are discussed.
This conference was the only opportunity for representatives of participating centers to gather and discuss several issues regarding the operation of the network database. Addition or modification of registered variables must also be discussed and determined at the conference.
All participating centers had the right to use the network database for their own research purposes. All accumulated data can be provided to the primary investigator at each center with an official application. As the number of registered infants increased and outcome data became available, the analysis data from the database were sent to many international publications. The first publication was made in 2005 [4], and since then, much data have been published in international journals [5], which eventually demonstrated the excellence of neonatal care in Japan. Figure 2 presents the number of publications and their cumulative number.
As the number of published manuscripts in the database increased, many questions regarding procedures and treatments in Japanese NICUs were received from outside Japan. Therefore, the manual titled ŌĆ£Neonatal intensive care manual for infants born less than 28 weeks of gestationŌĆØ was published and posted on the website in 2019 [6]. Once the manual was published, the similarities and differences in the procedures and treatments for extremely preterm infants became clear. Sharing and exchanging information within and among countries is another approach to improving outcomes in high-risk infants.
Acknowledgments
The author would like to thank all participating hospitals and infants involved in the study for their valuable contributions.
Figure┬Ā1.
Cumulative number of infants registered. This figure presents the cumulative number of infants registered in the database between 2003 and 2022. Currently, >80,000 infants are registered annually.
Figure┬Ā2.
Number of publications each year and total publications. This figure presents the number of publications in international journals published in English. Since the first publication in 2005, the number of publications has increased annually, and the total number of publications is almost 100.

REFERENCES
1. Kusuda S. Neonatal Research Network Database Japan [Internet]. Tokyo:NRN; 2022 [cited 2023 Feb 23]. Available from: http://plaza.umin.ac.jp/nrndata/indexe.htm.
2. Kusuda S, Fujimura M. Neonatal network database operated by the Neonatal Research Network of Japan. Pediatr Med 2021 [Epub]. https://dx.doi.org/10.21037/pm-21-71.

3. Neonatal Research Network Database Japan. Center list [Internet]. Tokyo:NRN; 2022 [cited 2023 Feb 23]. Available from: http://plaza.umin.ac.jp/nrndata/data/centerlist.xlsx.
4. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, et al. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics 2006;118:e1130ŌĆō8.



5. Neonatal Research Network Database Japan. 4/1/2022 (86 publications) [Internet]. Tokyo:NRN; 2022 [cited 2023 Feb 23]. Available from: http://plaza.umin.ac.jp/nrndata/pdf/publicationlist.pdf.
6. Neonatal Research Network Database Japan. Neonatal intensive care manual for the infants born less than 28 weeks of gestation (ver. 1.1) [Internet]. Tokyo:NRN; 2019 [cited 2023 Feb 23]. Available from: http://plaza.umin.ac.jp/nrndata/pdf/NICUManual.pdf.
-
METRICS

-
- 0 Crossref
- 1,331 View
- 38 Download
- Related article in NM
-
Early Neonatal Respiratory Morbidities in Term Neonates.2015 February;22(1)