|
 |
- Search
| Neonatal Med > Volume 30(4); 2023 > Article |
|
Abstract
Teratomas are the most common congenital tumors and contain cells from the ectoderm, mesoderm, and endoderm. They are mainly located in the central axis of the body. The tumors are most commonly found in the sacrococcygeal region, followed by the gonadal site and mediastinum, and rarely in the head and neck. Teratomas can cause various clinical symptoms depending on the location of the mass and may result in feeding difficulties or respiratory distress. We present a case of oropharyngeal teratoma accompanied by respiratory distress and persistent feeding difficulties, leading to compression of the temporomandibular joint, which in turn caused subluxation.
Teratomas are common congenital tumors with an incidence of 1 in 4,000 live births. However, oropharyngeal teratoma (OPT), also known as epignathus, is an extremely rare congenital teratoma with an incidence of 1 in 35,000 to 1 in 200,000 live births [1,2]. The bulk tumor mass often obstructs the oral cavity, resulting in life-threatening airway blockage and feeding problems, contributing to high mortality and morbidity rates during the perinatal period. OPT is usually associated with polyhydramnios and can be prenatally diagnosed using ultrasonography. We present a case of OPT associated with temporomandibular joint (TMJ) subluxation, cleft palate, and tongue anomalies. This rare disease’s clinical characteristics, diagnosis, and treatment are also reviewed.
The mother received regular antenatal care from a local obstetrician without significant problems. However, at 35 weeks of gestation, the patient was transferred to our hospital with sonographically diagnosed polyhydramnios. At 35+2 weeks of gestation, a planned cesarean section was performed, resulting in the birth of a female infant weighing 2,080 g. The Apgar scores were 6 and 7 at 1 and 5 minutes, respectively. During initial management in the delivery room, a large oral cavity mass was found, and the infant was admitted to the neonatal intensive care unit of Ajou University.
During the physical examination, the mouth could not be completely closed. When viewing the face from the front, the heights of both TMJ differed by more than 1 cm, and a noticeable asymmetry was observed. Consequently, a detailed inspection of the oral cavity was not possible because of the limited motion of the TMJ. A laryngoscopy revealed an OPT on the right side of the tongue. No anomalies were found in other parts of the body. The patient exhibited intermittent chest retraction with inspiratory stridor, which the mass may have caused. The infant remained stable with 25% (7 L) of high-flow nasal cannula therapy and maintained stable vital signs, including oxygen saturation. However, the infant experienced intermittent episodes of desaturation caused by regurgitation and aspiration during feeding that were transitioned to room air. Therefore, a gavage tube was inserted to continue oxygen therapy.
Initial blood examination results, including arterial blood gas analysis, were insignificant. Chest radiography revealed no abnormalities. Echocardiography showed a 2.5 mm sized muscular ventricular septal defect and a 2.4 mm sized atrial septal defect, with no hemodynamic significance. Laryngoscopy revealed a mass on the right side at the base of the tongue. Neck computed tomography (CT) showed a 2.8 cm calcified mass in the right oropharynx, resulting in compression of the internal jugular vein and posterolateral displacement of the internal carotid artery (Figure 1A). Neck magnetic resonance imaging (MRI) showed a 3.6×1.8×2 cm-sized heterogeneous mass in the right oropharynx with multiple tooth-like masses (Figure 1B). Right TMJ subluxation was also observed on facial 3D CT (Figure 2). Fortunately, there was no evidence of mass invasion into the brain parenchyma or cerebrospinal space on the brain MRI.
On hospital day 41, the mass was surgically removed under general endotracheal anesthesia (Figure 3A, B). Owing to limited intraoral access because of TMJ subluxation, only a partial amount of the teratoma was initially removed. Postoperatively, a cleft palate was observed beneath the mass (Figure 3C). The resected mass was round and white, measuring approximately 3.5×2.5×1.4 cm (Figure 4). The histology of the mass confirmed a mature teratoma containing keratinized squamous epithelium, glandular epithelium, and a bony structure (Figure 5).
The infant underwent rehabilitation therapy to improve mastication and swallowing function. Subluxation of the TMJ was corrected after complete resection. In a videofluoroscopic swallowing study (VFSS) conducted immediately after surgical removal, 40% of bottle feeding demonstrated effective swallowing, whereas 60% exhibited nasal regurgitation. However, following rehabilitation, the infant could consume liquids and solid food without exhibiting signs of aspiration or penetration into the oral cavity, pharynx, or esophagus, as observed during VFSS evaluation.
Teratomas are among the most frequent congenital tumors originating from germ cells, representing approximately 3% of all childhood malignancies. These tumors are distributed along the body’s midline, from the head to the coccyx. The coccyx region accounts for approximately 40% of cases, while head and neck tumors comprise 2% to 9% [3].
Malformations that occur in the oropharyngeal cavity of newborns are known as epignathus. Palatal, craniofacial, and cerebral malformations may accompany OPT [4]. A cleft palate is the malformation most commonly associated with epignathus, with an incidence of 6% to 20% [5]. Additionally, split tongue and craniofacial anomalies, including corpus callosum abnormalities, are commonly observed [6]. These anomalies can lead to generalized upper airway obstruction, respiratory failure, and feeding difficulties. These observations indicate that teratomas within the neck’s central region have the potential to grow in size and are associated with a poor prognosis [7]. In this case, the teratoma was located at the root of the right tongue, the respiratory distress was relatively mild, and the patient showed improvement with a highflow nasal cannula. The infant was presented with a cleft palate and a split tongue. These intraoral anomalies likely contribute to feeding difficulties, primarily by interfering with proper sucking. Approximately 67% of children affected by cleft palate report encountering feeding difficulties [8].
If the teratoma is large, it can be detected using antenatal ultrasonography. In this case, the patient’s mother was diagnosed with polyhydramnios using ultrasonography. This condition is likely attributable to an intraoral mass, which appears to compromise the fetus’s normal aspiration of amniotic fluid. It has been reported that polyhydramnios because of obstruction can occur in as many as 30% of cases [9].
Postnatal diagnosis of this condition can be achieved using CT or MRI. These diagnostic modalities help ascertain the precise location and dimensions of the tumor, as well as its potential intracranial infiltration. Approximately 50% of teratomas are calcified and may contain osteoid material [10]. In this case, there was no other vascular or intracranial involvement with calcification or dental components. Additionally, an oropharyngeal mass can cause structural issues because of its mass effect, including compression of the internal jugular vein and posterolateral displacement of the internal carotid artery. Subluxation of the right TMJ is also observed. TMJ diseases, which encompass congenital and developmental alterations, can include hypoplasia and aplasia of joint structures and require long-term rehabilitation [11].
Most teratomas are benign and can be treated by surgical excision [12]. In this case, the infant had limited access because of TMJ subluxation; therefore, partial resection was performed, and a second surgery was required. The clinical improvement suggests that surgical removal may have partially relieved the TMJ subluxation and that rehabilitation would have been beneficial. The infant showed improvements in eating and swallowing. She could seal her lips, control tongue movements, chew food on her own, drink liquids from a straw, and eat baby foods from a spoon.
We present a case of a rare tumor in the oropharynx of a neonate with respiratory distress and feeding difficulties. In the present case, the location of the teratoma at the base of the right tongue did not immediately cause severe respiratory tract obstruction at birth. However, a teratoma, concomitant cleft palate, palatal deformity, or subluxation of the TMJ may result in feeding difficulties in infants. In other words, the presence of TMJ subluxation set this case apart from the typical presentation because of the mass effect caused by the tumor’s particular location and size. The procedure was performed in two stages because of the surgical complexity associated with this condition. However, with consistent rehabilitation efforts, the functionality was restored to make liquid and solid diets feasible.
Nevertheless, it is imperative to emphasize the importance of ongoing reevaluation and continuous follow-up. Our clinical experience demonstrates a potential association between feeding difficulties and underlying anatomical anomalies in the oral cavity and upper respiratory tract. This case emphasizes the importance of identifying and understanding such anatomical anomalies, as they can significantly contribute to feeding difficulties and affect the overall well-being of infants. Timely recognition and appropriate management are essential for optimizing feeding abilities and promoting the healthy development of affected neonates. This report aimed to raise awareness among healthcare professionals regarding the significance of investigating anatomical factors in neonatal feeding difficulties, ultimately enhancing the quality of care provided to vulnerable patients.
ARTICLE INFORMATION
Ethical statement
This study was approved by the Institutional Review Board (AJOUIRB-EX-2023-411) of Ajou University Hospital. The requirement for written informed consent was waived because of the retrospective nature of the study.
Figure 1.
(A) A heterogeneous mass measuring 3.6×1.8×2 cm in size is located at the right oropharynx on computed tomography (arrow) and (B) composed of a tooth-like structure on magnetic resonance imaging (arrowheads).
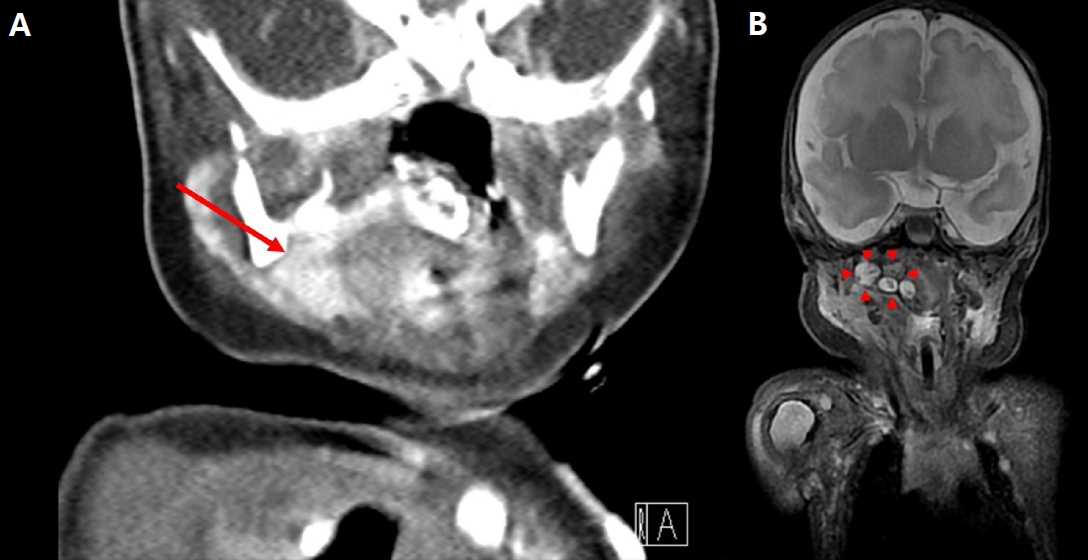
Figure 2.
(A, B) The right (Rt) condylar process was deviated, and the mandibular fossa demonstrated hypoplasia (arrows). (C) Facial computed tomography showed a subluxation of the temporomandibular joint (arrowheads). Abbreviation: Lt, left.

Figure 3.
(A) A mass was seen in the right oropharyngeal region (arrow). (B) The oropharyngeal mass was then fully exposed, and part of the mass was removed (arrowheads). (C) Abnormalities of the tongue, such as a fissured tongue and accessory tongue, were observed, along with cleft palate (large arrow).
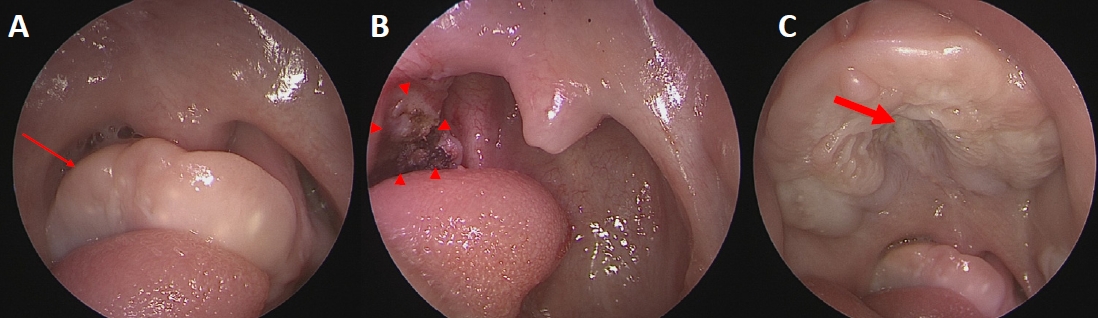
Figure 5.
The biopsy results indicated the presence of a keratinizing squamous epithelial-lining lesion in the right oropharynx. It was eventually diagnosed as a mature teratoma (H&E stain, ×20).

REFERENCES
1. Chiloiro S, Giampietro A, Bianchi A, De Marinis L. Clinical management of teratoma, a rare hypothalamic-pituitary neoplasia. Endocrine 2016;53:636–42.



2. Demajumdar R, Bhat N. Epignathus: a germ-cell tumour presenting as neonatal respiratory distress. Int J Pediatr Otorhinolaryngol 1999;47:87–90.


3. Acierno SP, Waldhausen JH. Congenital cervical cysts, sinuses and fistulae. Otolaryngol Clin North Am 2007;40:161–76.


4. Levine AB, Alvarez M, Wedgwood J, Berkowitz RL, Holzman I. Contemporary management of a potentially lethal fetal anomaly: a successful perinatal approach to epignathus. Obstet Gynecol 1990;76(5 Pt 2): 962–6.

5. Jayagobi PA, Chandran S, Sriram B, Chang KT. Ex-utero intrapartum treatment (EXIT) procedure for giant fetal epignathus. Indian Pediatr 2015;52:893–5.



6. Bale PM, Reye RD. Epignathus, double pituitary and agenesis of corpus callosum. J Pathol 1976;120:161–4.


7. April MM, Ward RF, Garelick JM. Diagnosis, management, and follow-up of congenital head and neck teratomas. Laryngoscope 1998;108:1398–401.


8. de Vries IA, Breugem CC, van der Heul AM, Eijkemans MJ, Kon M, Mink van der Molen AB. Prevalence of feeding disorders in children with cleft palate only: a retrospective study. Clin Oral Investig 2014;18:1507–15.
9. Enepekides DJ. Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am 2001;9:131–45.


10. Wiatrak BJ, Myer CM 3rd, Bratcher GO. Report of a nasopharyngeal teratoma evaluated with magnetic resonance imaging. Otolaryngol Head Neck Surg 1990;102:186–90.



-
METRICS

-
- 0 Crossref
- 671 View
- 21 Download
- Related articles in NM
-
A Case of Goldenhar Syndrome Associated with Holoprosencephaly1996 November;3(2)